Bioengineer Dr Alys Clark is building a virtual pregnancy model – a world first – to help with both detecting and monitoring risk during pregnancy.
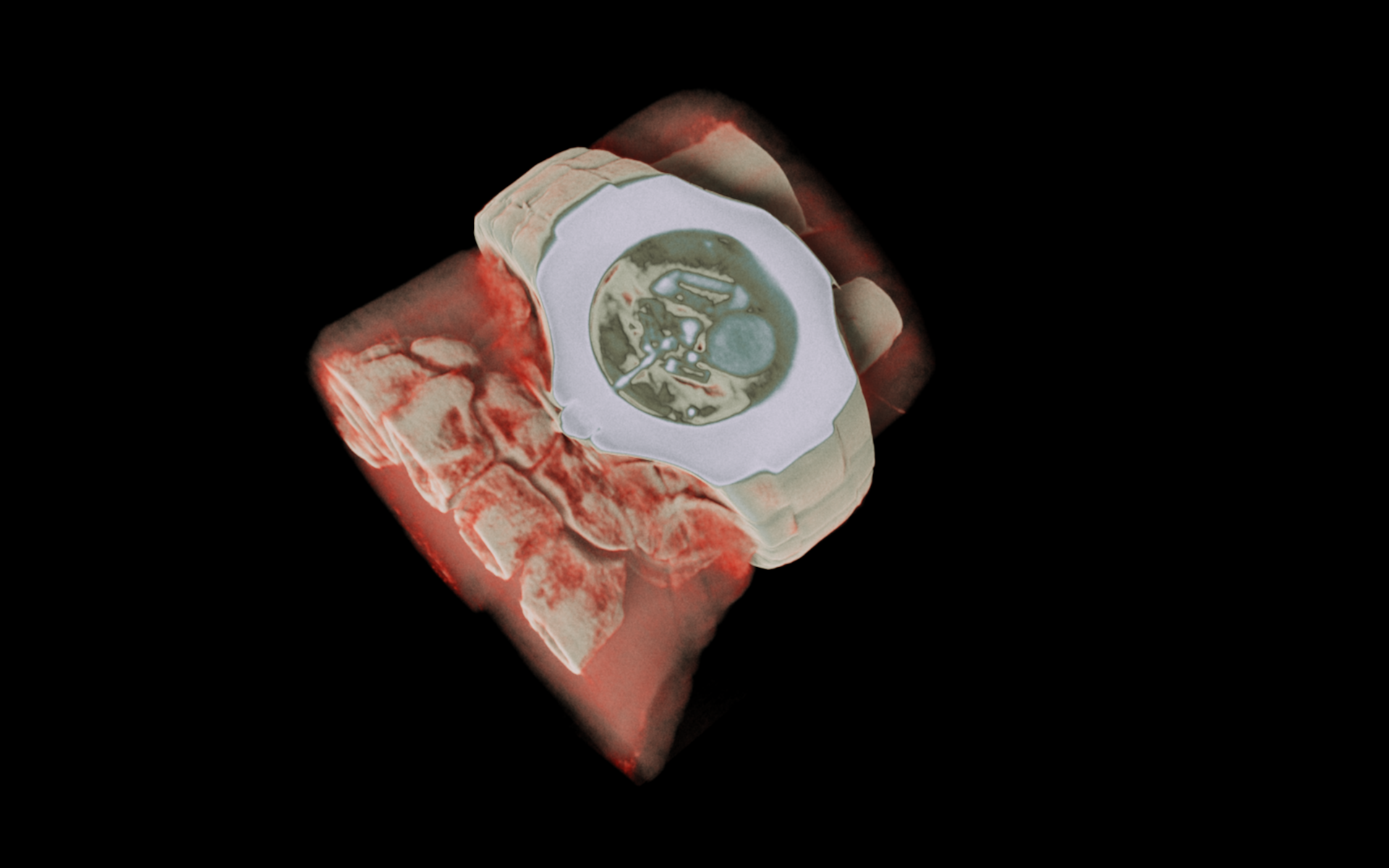
The goal is a new kind of atlas – a computational atlas that combines anatomy and function of the entire uterus and fetus during pregnancy. While researchers around the world are studying aspects of this system during pregnancy, the model Clark and her team is world-leading in its scope and coverage of the whole uterus.
“We’re trying to model the mother, fetus, and the blood flow within the placenta to understand what happens when that blood flow fails, something that can lead to fetal growth restriction where babies are born abnormally small or may even be stillborn,” says Dr Clark.
Poor placenta function is seen in one out of every 10 pregnancies, affecting more than 30,000 pregnancies each across New Zealand and Australia. Babies with fetal growth restriction are four times more likely to be stillborn.
Dr Clark and colleague Dr Jo James from the University of Auckland’s Faculty of Medical Health and Sciences are working internationally, including with researchers from Manchester, Oxford and Cambridge Universities to study how minor and major blood vessels in the uterus contribute to blood flow to the placenta. “If we can detect and monitor that blood flow from early on in the pregnancy, then we can halve the risk of stillbirths.”
The virtual model will also enable non-invasive monitoring, something that is critical given the rapid changes in physiology in both the mother and fetus. “A lot of medical technology such as CT scans and surgery can’t be used during pregnancy, but we can run the model using different datasets to predict or explain changes during pregnancy. That gives us a much better picture of what we should be looking for at 12-week and 20-week ultrasound scans.
“This means we can eliminate women with low risk and focus care on those with higher risk, and which is important in the case of pregnancy issues like fetal growth restriction where we miss around 50 per cent of them by the time of birth.”
The model is the result of more than 10 years’ work. “Models of other systems, such as adult health, the heart and the lung have been around for longer, but the evolution of pregnancy models has been slower,” says Dr Clark.
“It’s only in the last 10 years that we’ve started to see the transition from paper-based knowledge to technology. We now have the technology to create more detailed and higher resolution clinical datasets and non-invasive monitoring. We need to move on from historic and coarse measurements of fetal health such as the length of a leg or the circumference of the head.”
The next step is to discover how to incorporate data from healthy pregnancies and unhealthy pregnancies into the model and how the model can be translated into clinical practice. The ultimate goal is to build a cohort of virtual pregnancies from real data that predicts risk to mother and/or fetus.
Where to from here? Dr Clark talks about virtual trials, integrating data from wearables and continuous monitoring rather than time-restricted clinic visits.
Alys Clark obtained her Bachelor of Arts (Honours) in Mathematical Sciences from the University of Oxford and her Masters and PhD degrees in Applied Mathematics at the University of Adelaide. She joined the ABI in 2008 as a Postdoctoral Research Fellow in the Lung Research Group and is now one of the lead researchers in that group, as well as leading an active research group in reproductive health and development. She received a RSNZ Rutherford Discovery Fellowship in 2014, and the JH Michell Medal for Applied Mathematics in 2017.

.jpg)